Ganciclovir: Package Insert / Prescribing Info
Package insert / product label
Generic name: ganciclovir sodium
Dosage form: injection, powder, lyophilized, for solution
Drug class: Purine nucleosides
Medically reviewed by Drugs.com. Last updated on Jul 7, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- References
- How Supplied/Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
GANCICLOVIR for Injection, USP for intravenous use
Initial U.S. Approval: 1989
WARNING: HEMATOLOGIC TOXICITY, IMPAIRMENT OF FERTILITY, FETAL TOXICITY, MUTAGENESIS AND CARCINOGENESIS
See full prescribing information for complete boxed warning.
- Hematologic Toxicity: Granulocytopenia, anemia, thrombocytopenia, and pancytopenia have been reported in patients treated with ganciclovir ( 5.1).
- Impairment of Fertility: Based on animal data and limited human data, Ganciclovir for Injection, USP may cause temporary or permanent inhibition of spermatogenesis in males and suppression of fertility in females ( 5.3).
- Fetal Toxicity: Based on animal data, Ganciclovir for Injection, USP has the potential to cause birth defects in humans ( 5.4).
- Mutagenesis and Carcinogenesis: Based on animal data, Ganciclovir for Injection, USP has the potential to cause cancer in humans ( 5.5).
Indications and Usage for Ganciclovir
Ganciclovir for Injection, USP is a deoxynucleoside analogue cytomegalovirus (CMV) DNA polymerase inhibitor indicated for the:
Ganciclovir Dosage and Administration
- Ganciclovir for Injection, USP is administered only intravenously. ( 2.1)
|
Dosage in Adult Patients with Normal Renal Function |
|
|
Treatment of CMV retinitis (2.3) |
Induction: 5 mg/kg (given intravenously at a constant rate over 1 hour) every 12 hours for 14 to 21 days. Maintenance: 5 mg/kg (given intravenously at a constant rate over 1 hour) once daily for 7 days per week, or 6 mg/kg once daily for 5 days per week. |
|
Prevention of CMV disease in transplant recipients (2.4) |
Induction: 5 mg/kg (given intravenously at a constant rate over 1 hour) every 12 hours for 7 to 14 days. Maintenance: 5 mg/kg (given intravenously at a constant rate over 1 hour) once daily for 7 days per week, or 6 mg/kg once daily for 5 days per week until 100 to 120 days post-transplantation. |
- Adults with renal impairment: Adjust dosage based on creatinine clearance. ( 2.5)
Dosage Forms and Strengths
For injection: 500 mg of ganciclovir as lyophilized powder in a single-dose vial for reconstitution. ( 3)
Contraindications
- Hypersensitivity to ganciclovir or valganciclovir. ( 4)
Warnings and Precautions
- Renal Impairment: Increased serum creatinine levels have been observed with the use of ganciclovir, particularly in elderly patients and transplant recipients receiving concomitant nephrotoxic drugs. Monitor renal function during therapy with ganciclovir for injection, particularly in elderly patients and in patients taking other nephrotoxic drugs, and reduce dosage in patients with renal impairment. ( 5.2)
Adverse Reactions/Side Effects
Most common adverse reactions and laboratory abnormalities reported in at least 20% of patients were: pyrexia, diarrhea, leukopenia, nausea, anemia, asthenia, headache, cough, decreased appetite, dyspnea, abdominal pain, sepsis, hyperhidrosis, and blood creatinine increased. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Slate Run Pharmaceuticals, LLC at 1-888-341-9214 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Imipenem-cilastatin: Seizures were reported in patients receiving ganciclovir and imipenem-cilastatin. Concomitant use is not recommended unless the potential benefits outweigh the risks. ( 7)
- Cyclosporine or amphotericin B: When coadministered with ganciclovir, the risk of nephrotoxicity may be increased. Monitor renal function. ( 5.2, 7)
- Mycophenolate mofetil (MMF): When coadministered with ganciclovir, the risk of hematological and renal toxicity may be increased. Monitor for ganciclovir and MMF toxicity. ( 7)
- Other drugs associated with myelosuppression or nephrotoxicity: Due to potential for increased toxicity, such drugs should be considered for concomitant use with ganciclovir only if the potential benefits are judged to outweigh the risks. ( 7)
- Didanosine: Ganciclovir coadministered with didanosine may increase didanosine levels. Monitor for didanosine toxicity (e.g., pancreatitis). ( 7)
- Probenecid: May increase ganciclovir levels. Monitor for evidence of ganciclovir toxicity.
Use In Specific Populations
Lactation: Breastfeeding is not recommended with use of Ganciclovir for Injection, USP. ( 8.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 9/2024
Full Prescribing Information
WARNING: HEMATOLOGIC TOXICITY, IMPAIRMENT OF FERTILITY, FETAL TOXICITY, MUTAGENESIS AND CARCINOGENESIS
- Hematologic Toxicity: Granulocytopenia, anemia, thrombocytopenia, and pancytopenia have been reported in patients treated with ganciclovir [see Warnings and Precautions (5.1)] .
- Impairment of Fertility: Based on animal data and limited human data, Ganciclovir for Injection, USP may cause temporary or permanent inhibition of spermatogenesis in males and suppression of fertility in females [see Warnings and Precautions (5.3)] .
- Fetal Toxicity: Based on animal data, Ganciclovir for Injection, USP has the potential to cause birth defects in humans [see Warnings and Precautions (5.4)] .
- Mutagenesis and Carcinogenesis: Based on animal data, Ganciclovir for Injection, USP has the potential to cause cancers in humans [see Warnings and Precautions (5.5)] .
1. Indications and Usage for Ganciclovir
1.1 Treatment of CMV Retinitis
Ganciclovir for Injection, USP is indicated for the treatment of cytomegalovirus (CMV) retinitis in immunocompromised adult patients, including patients with acquired immunodeficiency syndrome (AIDS) [see Clinical Studies (14.1)].
1.2 Prevention of CMV Disease in Transplant Recipients
Ganciclovir for Injection, USP is indicated for the prevention of CMV disease in adult transplant recipients at risk for CMV disease [see Clinical Studies (14.2)].
2. Ganciclovir Dosage and Administration
2.1 Important Dosing and Administration Information
- To avoid phlebitis/pain at the infusion site, ganciclovir for injection must only be administered by intravenous infusion over 1 hour, preferably via plastic cannula, into a vein with adequate blood flow to permit rapid dilution and distribution.
- Do not administer ganciclovir for injection by rapid or bolus intravenous injection which may increase toxicity as a result of excessive plasma levels.
- The recommended dosage and infusion rate for ganciclovir for injection should not be exceeded.
- Do not administer the reconstituted ganciclovir for injection solution intramuscularly or subcutaneously because it may result in severe tissue irritation due to high pH [see Description 11].
- Administration of ganciclovir for injection should be accompanied by adequate hydration.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
2.2 Testing Before and During Treatment
- Females of reproductive potential should undergo pregnancy testing before initiation of treatment with ganciclovir for injection [see Warnings and Precautions (5.4), Use in Specific Populations (8.1, 8.3)].
- Complete blood counts with differential and platelet counts should be performed frequently, especially in patients in whom ganciclovir or other nucleoside analogues have previously resulted in cytopenias, or in whom absolute neutrophil counts are less than 1000 cells/μL at the beginning of treatment [see Warnings and Precautions (5.1)].
- All patients should be monitored for renal function before and during treatment with ganciclovir for injection and dose should be adjusted as needed [see Dosage and Administration (2.5), Warnings and Precautions (5.2)].
- Patients with CMV retinitis should have frequent ophthalmological examinations during treatment with ganciclovir for injection to monitor disease status and for other retinal abnormalities [see Adverse Reactions (6.1)].
2.3 Recommended Dosage for Treatment of CMV Retinitis in Adult Patients with Normal Renal Function
2.4 Recommended Dosage for Prevention of CMV Disease in Adult Transplant Recipients with Normal Renal Function
2.5 Recommended Dosage in Adult Patients with Renal Impairment
For patients with impairment of renal function, refer to Table 1for recommended doses of ganciclovir for injection for induction and maintenance dosage for treatment of CMV retinitis and prevention of CMV disease in recipients. Carefully monitor serum creatinine or creatinine clearance before and during treatment to allow for dosage adjustments in patients with impaired renal function.
|
||||
|
Creatinine Clearance*(mL/min) |
Ganciclovir for Injection Induction Dose (mg/kg) |
Dosing Interval (hours) for Induction |
Ganciclovir for Injection Maintenance Dose (mg/kg) |
Dosing Interval (hours) for Maintenance |
|
Greater than or equal to 70 |
5 |
12 |
5 |
24 |
|
50-69 |
2.5 |
12 |
2.5 |
24 |
|
25-49 |
2.5 |
24 |
1.25 |
24 |
|
10-24 |
1.25 |
24 |
0.625 |
24 |
|
Less than 10 |
1.25 |
3 times per week, following hemodialysis |
0.625 |
3 times per week, following hemodialysis |
Patients Undergoing Hemodialysis
Induction dosing for ganciclovir for injection in patients undergoing hemodialysis should not exceed 1.25 mg/kg 3 times per week; and maintenance dosing should not exceed 0.625 mg/kg 3 times per week following each hemodialysis session. Ganciclovir for injection should be given shortly after completion of the hemodialysis session, since hemodialysis has been shown to reduce plasma levels by approximately 50% [see Clinical Pharmacology (12.3)].
2.6 Preparation of Ganciclovir Injection, USP
- Ganciclovir for Injection, USP must be reconstituted and diluted under the supervision of a healthcare provider and administered as intravenous infusion. Each 10 mL clear glass vial contains 543 mg ganciclovir sodium equivalent to 500 mg of ganciclovir. Wearing disposable gloves is recommended during reconstitution and when wiping the outer surface of the vial and the table after reconstitution. The contents of the vial should be prepared for administration in the following manner:
- Reconstitution Instructions:
- Reconstitute lyophilized Ganciclovir for Injection, USP by injecting 10 mL of Sterile Water for Injection, USP, into the vial. Do not use bacteriostatic water for injection containing parabens. It is incompatible with Ganciclovir for Injection, USP and may cause precipitation.
- Gently swirl the vial in order to ensure complete wetting of the product. Continue swirling until a clear reconstituted solution is obtained.
- Visually inspect the reconstituted solution for particulate matter and discoloration prior to proceeding with infusion. Discard the vial if particulate matter or discoloration is observed.
- Reconstituted solution in the vial is stable at room temperature (25°C (77°F)) for 12 hours. Do not refrigerate or freeze. Discard any unused portion of the reconstituted solution.
- Infusion Instructions:
- Based on patient weight, the appropriate volume of the reconstituted solution (ganciclovir concentration 50 mg/mL) should be removed from the vial and added to an acceptable infusion fluid (typically 100 mL) for delivery over the course of 1 hour. Infusion concentrations greater than 10 mg/mL are not recommended. The following infusion fluids have been determined to be chemically and physically compatible with Ganciclovir for Injection, USP solution: 0.9% Sodium Chloride, 5% Dextrose, Ringer’s Injection and Lactated Ringer’s Injection, USP.
- Ganciclovir for Injection, USP, when reconstituted with Sterile Water for Injection (non-bacteriostatic) and further diluted with 0.9% sodium chloride injection or other acceptable infusion fluid as specified above, should be used within 24 hours of dilution to reduce the risk of bacterial contamination. The diluted infusion solution should be refrigerated (2°C to 8°C (36° to 46°F)). Do not freeze.
2.7 Handling and Disposal
Caution should be exercised in the handling and preparation of solutions of Ganciclovir for Injection, USP. Solutions of Ganciclovir for Injection, USP are alkaline (pH 11). Avoid direct contact of the skin or mucous membranes with Ganciclovir for Injection, USP solution. If such contact occurs, wash thoroughly with soap and water; rinse eyes thoroughly with plain water. Wearing disposable gloves is recommended.
Because ganciclovir shares some of the properties of antitumor agents (i.e., carcinogenicity and mutagenicity), consideration should be given to handling and disposal according to guidelines issued for antineoplastic drugs 1. Discard any unused portion of the reconstituted solution [see How Supplied/Storage and Handling (16)].
3. Dosage Forms and Strengths
For injection: Single-dose vial containing 500 mg of ganciclovir as a sterile lyophilized white to off-white powder for reconstitution with 10 mL of preservative-free sterile water for injection, USP for intravenous use. The concentration of ganciclovir in the reconstituted solution is 50 mg/mL [see Dosage and Administration (2.6)].
4. Contraindications
Ganciclovir for Injection, USP is contraindicated in patients who have experienced a clinically significant hypersensitivity reaction (e.g., anaphylaxis) to ganciclovir, valganciclovir or any component of the formulation.
5. Warnings and Precautions
5.1 Hematologic Toxicity
Granulocytopenia (neutropenia), anemia, thrombocytopenia and pancytopenia, have been observed in patients treated with ganciclovir. The frequency and severity of these events vary widely in different patient populations [see Adverse Reactions (6.1)]. Ganciclovir for injection is not recommended if the absolute neutrophil count is less than 500 cells/μL, hemoglobin is less than 8 g/dL, or the platelet count is less than 25,000 cells/μL. Ganciclovir for injection should also be used with caution in patients with pre-existing cytopenias and in patients receiving myelosuppressive drugs or irradiation. Granulocytopenia (neutropenia) usually occurs during the first or second week of treatment but may occur at any time during treatment. Cell counts usually begin to recover within 3 to 7 days after discontinuing drug. Colony-stimulating factors have been shown to increase neutrophil and white blood cell counts in patients receiving ganciclovir solution for treatment of CMV retinitis.
Due to the frequency of neutropenia, anemia and thrombocytopenia in patients receiving ganciclovir for injection [see Adverse Reactions (6.1)], complete blood counts with differential and platelet counts should be performed frequently in all patients, especially in patients with renal impairment and in patients in whom ganciclovir or other nucleoside analogues have previously resulted in leukopenia, or in whom neutrophil counts are less than 1000 cells/µL at the beginning of treatment [see Dosage and Administration (2.2)].
5.2 Renal Impairment
Ganciclovir for injection should be used with caution in patients with impaired renal function because the half-life and plasma/serum concentrations of ganciclovir will be increased due to reduced renal clearance. If renal function is impaired, dosage adjustments are recommended [see Dosage and Administration (2.5), Use in Specific Populations (8.5)].
Increased serum creatinine levels have been reported in elderly patients and in transplant recipients receiving concomitant nephrotoxic medications (i.e., cyclosporine and amphotericin B). Monitoring renal function during therapy with ganciclovir for injection is essential, especially for elderly patients and those patients receiving concomitant agents that may cause nephrotoxicity [see Dosage and Administration (2.5), Drug Interactions (7), Use in Specific Populations (8.5)].
5.3 Impairment of Fertility
Based on animal data and limited human data, ganciclovir for injection at the recommended human dose (RHD) may cause temporary or permanent inhibition of spermatogenesis in males, and may cause suppression of fertility in females. Advise patients that fertility may be impaired with the use of ganciclovir for injection [see Use in Specific Population (8.1, 8.3), Nonclinical Toxicology (13.1)].
5.4 Fetal Toxicity
Ganciclovir for injection may cause fetal toxicity when administered to pregnant women based on findings in animal studies. Systemic exposure of ganciclovir in animals at approximately 2 times the RHD caused fetal growth retardation, embryolethality, teratogenicity, and/or maternal toxicity. Teratogenic changes in animals included cleft palate, anophthalmia/microphthalmia, aplastic organs (kidney and pancreas), hydrocephaly and brachygnathia. Women of childbearing potential should be advised to use effective contraception during treatment and for at least 30 days following treatment with ganciclovir for injection. Similarly, men should be advised to practice barrier contraception during and for at least 90 days following treatment with ganciclovir for injection [see Use in Specific Populations (8.1, 8.3), Nonclinical Toxicology (13.1)].
5.5 Mutagenesis and Carcinogenesis
Animal data indicate that ganciclovir is mutagenic and carcinogenic. Ganciclovir for injection should therefore be considered a potential carcinogen in humans [see Dosage and Administration (2.7), Nonclinical Toxicology (13.1)].
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed in greater detail in other sections of the labeling:
- Hematologic Toxicity [see Warnings and Precautions (5.1)]
- Renal Impairment [see Warnings and Precautions (5.2)]
- Impairment of Fertility [see Warnings and Precautions (5.3)]
- Fetal Toxicity [see Warnings and Precautions (5.4)]
- Mutagenesis and Carcinogenesis [see Warnings and Precautions (5.5)]
6.1 Clinical Trial Experience in Adult Patients
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The most common adverse reactions and laboratory abnormalities reported in at least 20% of patients were pyrexia, diarrhea, leukopenia, nausea, anemia, asthenia, headache, cough, decreased appetite, dyspnea, abdominal pain, sepsis, hyperhidrosis, and blood creatinine increased.
Selected adverse reactions that occurred during clinical trials of ganciclovir are summarized below, according to the participating study patient population.
Adverse Reactions in Patients with CMV Retinitis
Three controlled, randomized, phase 3 trials comparing intravenous ganciclovir and ganciclovir capsules for maintenance treatment of CMV retinitis have been completed. During these trials, intravenous ganciclovir or ganciclovir capsules were prematurely discontinued in 9% of subjects because of adverse reactions. Selected adverse reactions and laboratory abnormalities reported during the conduct of these controlled trials are summarized in Table 2and Table 3, respectively [see Clinical Studies (14.1)].
|
Maintenance Treatment Studies |
||
|
Adverse Reaction |
Intravenous Ganciclovir (n=179) |
Ganciclovir Capsules (n=326) |
|
Pyrexia |
48% |
38% |
|
Diarrhea |
44% |
41% |
|
Leukopenia |
41% |
29% |
|
Anemia |
25% |
19% |
|
Total Catheter Events: |
22% |
6% |
|
Catheter Infection |
9% |
4% |
|
Catheter Sepsis |
8% |
1% |
|
Other Catheter Related Events |
5% |
1% |
|
Sepsis |
15% |
4% |
|
Decreased Appetite |
14% |
15% |
|
Vomiting |
13% |
13% |
|
Infection |
13% |
9% |
|
Hyperhidrosis |
12% |
11% |
|
Chills |
10% |
7% |
|
Neuropathy Peripheral |
9% |
8% |
|
Thrombocytopenia |
6% |
6% |
|
Pruritus |
5% |
6% |
Retinal Detachment
Retinal detachment has been observed in subjects with CMV retinitis both before and after initiation of therapy with ganciclovir. Its relationship to therapy with ganciclovir is unknown. Retinal detachment occurred in 11% of patients treated with intravenous ganciclovir and in 8% of patients treated with ganciclovir capsules.
|
CMV Retinitis Treatment* |
||
|
Laboratory Abnormalities |
Intravenous Ganciclovir† 5 mg/kg/day (N=175) % |
Ganciclovir Capsules‡ 3000 mg/day (N=320) % |
|
Neutropenia with Absolute Neutrophil Count (ANC) per μL: |
||
|
<500 |
25% |
18% |
|
500-<749 |
14% |
17% |
|
750-<1000 |
26% |
19% |
|
Anemia with Hemoglobin g/dL: |
||
|
<6.5 g/dL |
5% |
2% |
|
6.5-8.0 |
16% |
10% |
|
8.0-<9.5 |
26% |
25% |
|
Serum Creatinine mg/mL: |
||
|
≥2.5 |
2% |
1% |
|
≥1.5-<2.5 |
14% |
12% |
Adverse Reactions in Transplant Recipients
There have been three controlled clinical trials of intravenous ganciclovir for the prevention of CMV disease in transplant recipients. Selected laboratory abnormalities are summarized in Tables 4 and Table 5 below. Table 4shows the frequency of neutropenia and thrombocytopenia and Table 5shows the frequency of elevated serum creatinine values observed in these trials [see Clinical Studies (14.2)].
|
Laboratory Abnormalities |
Heart Allograft* |
Bone Marrow Allograft† |
||
|
Intravenous Ganciclovir (n=76) |
Placebo (n=73) |
Intravenous Ganciclovir (n=57) |
Control (n=55) |
|
|
Neutropenia Absolute Neutrophil Count (ANC) per μL: |
||||
|
<500 |
4% |
3% |
12% |
6% |
|
500-1000 |
3% |
8% |
29% |
17% |
|
TOTAL ANC ≤1000/μL |
7% |
11% |
41% |
23% |
|
Thrombocytopenia Platelet count per μL: |
||||
|
<25,000 |
3% |
1% |
32% |
28% |
|
25,000-50,000 |
5% |
3% |
25% |
37% |
|
TOTAL Platelet Count ≤50,000 μL |
8% |
4% |
57% |
65% |
|
Serum Creatinine Levels (mg/dL) |
Heart Allograft ICM 1496 |
Bone Marrow Allograft ICM 1570 |
Bone Marrow Allograft ICM 1689 |
|||
|
Intravenous Ganciclovir (n=76) |
Placebo (n=73) |
Intravenous Ganciclovir (n=20) |
Control (n=20) |
Intravenous Ganciclovir (n=37) |
Placebo (n=35) |
|
|
≥2.5 |
18% |
4% |
20% |
0% |
0% |
0% |
|
≥1.5-<2.5 |
58% |
69% |
50% |
35% |
43% |
44% |
Other Adverse Reactions in Clinical Trials in Patients with CMV Retinitis and in Transplant Recipients
Adverse drug reactions with intravenous ganciclovir or ganciclovir capsules in controlled clinical studies in either subjects with AIDS or transplant recipients are listed below [see Clinical Studies (14)]. All these events occurred in at least 3 subjects.
Blood and lymphatic disorders:pancytopenia, bone marrow failure
Cardiac disorders:arrhythmias
Ear and labyrinth disorders:tinnitus, ear pain, deafness
Eye disorders:visual impairment, vitreous disorders, eye pain, conjunctivitis, macular edema
Gastrointestinal disorders:nausea, abdominal pain, dyspepsia, flatulence, constipation, mouth ulceration, dysphagia, abdominal distention, pancreatitis, gastrointestinal perforation, eructation, dry mouth
General disorders and administration site conditions:fatigue, injection site inflammation, edema, pain, malaise, asthenia, chest pain, multiple organ failure
Immune system disorders:hypersensitivity
Infections and infestations:candida infections including oral candidiasis, upper respiratory infection, influenza, urinary tract infections, cellulitis
Investigations:blood alkaline phosphatase increased, hepatic function abnormal, aspartate aminotransferase increased, alanine aminotransferase increased, creatinine clearance decreased
Metabolism and nutrition disorders:weight decreased
Musculoskeletal and connective tissue disorders:back pain, myalgia, arthralgia, muscle spasms, leg cramps, myasthenia
Nervous system disorders:headache, insomnia, dizziness, paresthesia, hypoaesthesia, seizures, somnolence, dysgeusia (taste disturbance), tremor
Psychiatric disorders:depression, confusional state, anxiety, agitation, psychotic disorder, thinking abnormal, abnormal dreams
Renal and urinary disorders:kidney failure, renal function abnormal, urinary frequency, hematuria
Respiratory, thoracic and mediastinal disorders:increased cough, dyspnea
Skin and subcutaneous tissues disorders:dermatitis, alopecia, dry skin, urticaria, rash
Vascular disorders:hypotension, hypertension, phlebitis, vasodilation
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of intravenous ganciclovir or ganciclovir capsules. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic disorders:hemolytic anemia, agranulocytosis, granulocytopenia
Cardiac disorders:cardiac arrest, conduction disorder, torsade de pointes, ventricular tachycardia
Congenital, familial and genetic disorders:congenital anomaly
Endocrine disorders:inappropriate antidiuretic hormone secretion
Eye disorders:cataracts, dry eyes
Gastrointestinal disorders:intestinal ulcer
Hepatobiliary disorders:cholelithiasis, cholestasis, hepatic failure, hepatitis
Immune system disorders:anaphylactic reaction, allergic reaction, vasculitis
Investigations:blood triglycerides increased
Metabolism and nutrition disorders:acidosis, hypercalcemia, hyponatremia
Musculoskeletal and connective tissue disorders:arthritis, rhabdomyolysis
Nervous system disorders:dysesthesia, dysphasia, extrapyramidal disorder, facial paralysis, amnesia, anosmia, myelopathy, cerebrovascular accident, third cranial nerve paralysis, aphasia, encephalopathy, intracranial hypertension
Psychiatric disorders:irritability, hallucinations
Renal and urinary disorders:renal tubular disorder, hemolytic uremic syndrome
Reproductive system and breast disorders:infertility, testicular hypotrophy
Respiratory, thoracic and mediastinal disorders:bronchospasm, pulmonary fibrosis
Skin and subcutaneous tissues disorders:exfoliative dermatitis, Stevens-Johnson syndrome
Vascular disorders:peripheral ischemia
7. Drug Interactions
Drug-drug interaction studies were conducted in patients with normal renal function. Patients with impaired renal function may have increased concentrations of ganciclovir and the coadministered drug following concomitant administration of ganciclovir for injection and drugs excreted by the same pathway as ganciclovir. Therefore, these patients should be closely monitored for toxicity of ganciclovir and the coadministered drug.
Established and other potentially significant drug interactions conducted with ganciclovir are listed in Table 6[see Clinical Pharmacology (12.3)].
|
Name of the Concomitant Drug |
Change in the Concentration of Ganciclovir or Concomitant Drug |
Clinical Comment |
|
Imipenem-cilastatin |
Unknown |
Coadministration with imipenem-cilastatin is not recommended because generalized seizures have been reported in patients who received ganciclovir and imipenem-cilastatin. |
|
Cyclosporine or amphotericin B |
Unknown |
Monitor renal function when ganciclovir for injection is coadministered with cyclosporine or amphotericin B because of potential increase in serum creatinine [see Warnings and Precautions (5.2)]. |
|
Mycophenolate mofetil (MMF) |
↔Ganciclovir (in patients with normal renal function) ↔MMF (in patients with normal renal function) |
Based on increased risk, patients should be monitored for hematological and renal toxicity. |
|
Other drugs associated with myelosuppresion or nephrotoxicity (e.g., dapsone, doxorubicin, flucytosine, hydroxyurea, pentamidine, tacrolimus, trimethoprim/sulfamethoxazole, vinblastine, vincristine and zidovudine) |
Unknown |
Because of potential for higher toxicity, coadministration with ganciclovir for injection should be considered only if the potential benefits are judged to outweigh the risks. |
|
Didanosine |
↔ Ganciclovir ↑ Didanosine |
Patients should be closely monitored for didanosine toxicity (e.g., pancreatitis). |
|
Probenecid |
↑ Ganciclovir |
Ganciclovir for injection dose may need to be reduced. Monitor for evidence of ganciclovir toxicity. |
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
In animal studies, ganciclovir caused maternal and fetal toxicity and embryo-fetal mortality in pregnant mice and rabbits as well as teratogenicity in rabbits at exposures two times the exposure at the recommended human dose (RHD) [see Data]. Although placental transfer of ganciclovir has been shown to occur based on ex vivoexperiments with human placenta and in at least one case report in a pregnant woman, no adequate human data are available to establish whether ganciclovir for injection poses a risk to pregnancy outcomes. The background risk of major birth defects and miscarriage for the indicated populations is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in the clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo-Fetal Risk
Most maternal CMV infections are asymptomatic or they may be associated with a self-limited mononucleosis-like syndrome. However, in immunocompromised patients (i.e., transplant patients or patients with AIDS), CMV infections may be symptomatic and may result in significant maternal morbidity and mortality. The transmission of CMV to the fetus is a result of maternal viremia and transplacental infection. Perinatal infection can also occur from exposure of the neonate to CMV shedding in the genital tract. Approximately 10% of children with congenital CMV infection are symptomatic at birth. Mortality in symptomatic infants is about 10% and approximately 50 to 90% of symptomatic surviving newborns experience significant morbidity, including mental retardation, sensorineural hearing loss, microcephaly, seizures, and other medical problems. The risk of congenital CMV infection resulting from primary maternal CMV infection may be higher and of greater severity than that resulting from maternal reactivation of CMV infection.
Data
Animal Data
Daily intravenous doses of ganciclovir were administered to pregnant mice (108 mg/kg/day) and rabbits (60 mg/kg/day), and also to female mice (90 mg/kg) prior to mating, during gestation, and during lactation. Fetal resorptions were present in at least 85% of rabbits and mice. Additional effects observed in rabbits included fetal growth retardation, embryolethality, teratogenicity, and/or maternal toxicity. Teratogenic changes included cleft palate, anophthalmia/microphthalmia, aplastic organs (kidney and pancreas), hydrocephaly, and brachygnathia. In pre/postnatal development studies in mice, there were maternal/fetal toxicity and embryolethality which included fetal effects of hypoplasia of the testes and seminal vesicles in the male offspring, as well as pathologic changes in the nonglandular region of the stomach. The systemic exposure (AUC) of ganciclovir during these studies was approximately 2 times (pregnant mice and rabbits) and 1.7 times (pre/postnatal mice) the exposure in humans at the RHD [see Nonclinical Toxicology (13.1)].
8.2 Lactation
Risk Summary
No data are available regarding the presence of ganciclovir in human milk, the effects on the breastfed infant, or the effects on milk production. When ganciclovir was administered to lactating rats, ganciclovir was present in milk [see Data]. Advise nursing mothers that breastfeeding is not recommended during treatment with ganciclovir for injection because of the potential for serious adverse reactions in nursing infants [see Warnings and Precautions (5.1, 5.3, 5.4, 5.5), Nonclinical Toxicology (13.1)]. Furthermore, the Centers for Disease Control and Prevention recommends that HIV-infected mothers not breastfeed their infants to avoid potential postnatal transmission of HIV.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Females of reproductive potential should undergo pregnancy testing before initiation of treatment with ganciclovir for injection [see Dosage and Administration (2.2), Use in Specific Populations (8.1)].
Contraception
Females
Because of the mutagenic and teratogenic potential of ganciclovir, females of reproductive potential should be advised to use effective contraception during treatment and for at least 30 days following treatment with ganciclovir for injection [see Dosage and Administration (2.2), Warnings and Precautions (5.4), Nonclinical Toxicology (13.1)].
Males
Because of its mutagenic potential, males should be advised to practice barrier contraception during and for at least 90 days following treatment with ganciclovir for injection [see Warnings and Precautions (5.4), Nonclinical Toxicology (13.1)].
Infertility
Ganciclovir for injection at the recommended doses may cause temporary or permanent female and male infertility [see Warnings and Precautions (5.3), Nonclinical Toxicology (13.1)].
Data
Human Data
In a small, open-label, non-randomized clinical study, adult male renal transplant patients receiving valganciclovir (the prodrug of ganciclovir) for CMV prophylaxis for up to 200 days post-transplantation were compared to an untreated control group. Patients were followed-up for six months after valganciclovir discontinuation. Among 24 evaluable patients in the valganciclovir group, the mean sperm density at the end of treatment visit decreased by 11 million/mL from baseline; whereas, among 14 evaluable patients in the control group the mean sperm density increased by 33 million/mL. However, at the follow-up visit among 20 evaluable patients in the valganciclovir group, the mean sperm density was comparable to that observed among 10 evaluable patients in the untreated control group (the mean sperm density at the end of follow-up visit increased by 41 million/mL from baseline in the valganciclovir group and by 43 million/mL in the untreated group).
8.4 Pediatric Use
Safety and effectiveness of ganciclovir for injection have not been established in pediatric patients.
A total of 120 pediatric patients with serious CMV infections participated in clinical trials. Granulocytopenia and thrombocytopenia were the most common adverse reactions. The pharmacokinetic characteristics of ganciclovir after administration of ganciclovir for injection were studied in 27 neonates (aged 2 to 49 days) and 10 pediatric patients, aged 9 months to 12 years. In neonates, the pharmacokinetic parameters after ganciclovir intravenous doses of 4 mg/kg (n=14) and 6 mg/kg (n=13) were C max5.5 ± 1.6 and 7.0 ± 1.6 mcg/mL, systemic clearance 3.14 ± 1.75 and 3.56 ± 1.27 mL/min/kg, and t 1/2of 2.4 hours (harmonic mean) for both doses, respectively.
In pediatric patients 9 months to 12 years of age, the pharmacokinetic characteristics of ganciclovir were the same after single and multiple (every 12 hours) intravenous doses (5 mg/kg). The steady-state volume of distribution was 0.64 ± 0.22 L/kg, C maxwas 7.9 ± 3.9 mcg/mL, systemic clearance was 4.7 ± 2.2 mL/min/kg, and t 1/2was 2.4 ± 0.7 hours.
Although the pharmacokinetics of intravenous ganciclovir in pediatric patients were similar to those observed in adults, the safety and efficacy of ganciclovir at these exposures in pediatric patients have not been established.
8.5 Geriatric Use
Clinical studies of ganciclovir did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. Ganciclovir is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because renal clearance decreases with age, ganciclovir should be administered to elderly patients with special consideration of their renal status. Renal function should be monitored and dosage adjustments should be made accordingly [see Dosage and Administration (2.5), Warnings and Precautions (5.2), Use in Specific Populations (8.6)].
8.6 Renal Impairment
Dose reduction is recommended when administering ganciclovir for injection to patients with renal impairment [see Dosage and Administration (2.5), Warnings and Precautions (5.2)].
10. Overdosage
Reports of adverse reactions after overdoses with ganciclovir for injection, some with fatal outcomes, have been received from clinical trials and during post-marketing experience. One or more of the following adverse reactions has been reported with overdoses:
Hematological toxicity:myelosuppression including pancytopenia, leukopenia, neutropenia, granulocytopenia, thrombocytopenia, bone marrow failure
Hepatotoxicity:hepatitis, liver function disorder
Renal toxicity:worsening of hematuria in a patient with pre-existing renal impairment, acute kidney injury, elevated creatinine
Gastrointestinal toxicity:abdominal pain, diarrhea, vomiting
Neurotoxicity:seizure
Since ganciclovir is dialyzable, dialysis may be useful in reducing serum concentrations in patients who have received an overdose of ganciclovir [see Clinical Pharmacology (12.3)]. Adequate hydration should be maintained. The use of hematopoietic growth factors should be considered in patients with cytopenias [see Warnings and Precautions (5.1)].
11. Ganciclovir Description
Ganciclovir for injection contains ganciclovir, in the form of the sodium salt for intravenous injection. Ganciclovir is a synthetic guanine derivative active against cytomegalovirus (CMV).
Chemically, ganciclovir is 9-[[2-hydroxy-1-(hydroxymethyl)-ethoxy]methyl]guanine and ganciclovir sodium is 9-[[2-hydroxy-1-(hydroxymethyl)-ethoxy]methyl]guanine, monosodium salt. The chemical structures of ganciclovir sodium and ganciclovir are:
Ganciclovir is a white to off-white crystalline powder. Ganciclovir is a polar hydrophilic compound with a solubility of 2.6 mg/mL in water at 25°C and an n-octanol/water partition coefficient of 0.022. The pK as for ganciclovir are 2.2 and 9.4.
Ganciclovir for injection (ganciclovir), formulated as monosodium salt, using sodium hydroxide as a salt forming agent, is a sterile white to off-white lyophilized powder. The lyophilized powder has an aqueous solubility of greater than 50 mg/mL at 25°C. At physiological pH, ganciclovir sodium exists as the un-ionized form with a solubility of approximately 6 mg/mL at 37°C.
Each vial contains 543 mg ganciclovir sodium equivalent to 500 mg ganciclovir.
Inactive ingredients may include hydrochloric acid (QS) and sodium hydroxide (QS) added to adjust the pH.
All doses in this package insert are specified in terms of ganciclovir
12. Ganciclovir - Clinical Pharmacology
12.1 Mechanism of Action
Ganciclovir is an antiviral drug with activity against CMV [see Microbiology (12.4)].
12.3 Pharmacokinetics
Absorption
At the end of a 1-hour intravenous infusion of 5 mg/kg ganciclovir, total AUC ranged between 22.1 ± 3.2 (n=16) and 26.8 ± 6.1 mcg∙hr/mL (n=16) and C maxranged between 8.27 ± 1.02 (n=16) and 9.0 ± 1.4 mcg/mL (n=16).
Distribution
The steady-state volume of distribution of ganciclovir after intravenous administration was 0.74 ± 0.15 L/kg (n=98). Ganciclovir diffuses across the placenta. Cerebrospinal fluid concentrations obtained 0.25 to 5.67 hours post-dose in 3 patients who received 2.5 mg/kg ganciclovir intravenously every 8 hours or every 12 hours ranged from 0.31 to 0.68 mcg/mL, representing 24% to 70% of the respective plasma concentrations. Binding to plasma proteins was 1% to 2% over ganciclovir concentrations of 0.5 and 51 mcg/mL.
Elimination
When administered intravenously, ganciclovir exhibits linear pharmacokinetics over the range of 1.6 to 5.0 mg/kg. Renal excretion of unchanged drug by glomerular filtration and active tubular secretion is the major route of elimination of ganciclovir. In patients with normal renal function, 91.3 ± 5.0% (n=4) of intravenously administered ganciclovir was recovered unmetabolized in the urine. Systemic clearance of intravenously administered ganciclovir was 3.52 ± 0.80 mL/min/kg (n=98) while renal clearance was 3.20 ± 0.80 mL/min/kg (n=47), accounting for 91 ± 11% of the systemic clearance (n=47). Half-life was 3.5 ± 0.9 hours (n=98) following intravenous administration
Special Populations
Pharmacokinetics in Patients with Renal Impairment
The pharmacokinetics following intravenous administration of ganciclovir solution were evaluated in 10 immunocompromised patients with renal impairment who received doses ranging from 1.25 to 5.0 mg/kg. Decreased renal function results in decreased clearance of ganciclovir ( Table 7).
|
Estimated Creatinine Clearance (mL/min) |
n |
Dose |
Clearance (mL/min) Mean ± SD |
Half-life (hours) Mean ± SD |
|
50-79 |
4 |
3.2-5 mg/kg |
128 ± 63 |
4.6 ± 1.4 |
|
25-49 |
3 |
3-5 mg/kg |
57 ± 8 |
4.4 ± 0.4 |
|
<25 |
3 |
1.25-5 mg/kg |
30 ± 13 |
10.7 ± 5.7 |
Plasma concentrations of ganciclovir are reduced by about 50% during a 4 hour hemodialysis session.
Pharmacokinetics in Geriatric Patients
The pharmacokinetic profiles of ganciclovir in patients 65 years of age and older have not been established. As ganciclovir is mainly renally excreted and since renal clearance decreases with age, a decrease in ganciclovir total body clearance and a prolongation of ganciclovir half-life can be anticipated in patients 65 years of age and older [see Dosage and Administration (2.5), Use in Specific Populations (8.5)].
Drug Interaction Studies
Tables 8 and 9 provide a listing of established drug interaction studies with ganciclovir. Table 8provides the effects of coadministered drug on ganciclovir plasma pharmacokinetic parameters, whereas Table 9provides the effects of ganciclovir on plasma pharmacokinetic parameters of coadministered drug.
|
Coadministered Drug |
Ganciclovir Dosage |
N |
Ganciclovir Pharmacokinetic (PK) Parameter |
|
Mycophenolate mofetil (MMF) 1.5 g single dose |
5 mg/kg IV single dose |
12 |
No effect on ganciclovir PK parameters observed (patients with normal renal function) |
|
Trimethoprim 200 mg once daily |
1000 mg orally every 8 hours |
12 |
No effect on ganciclovir PK parameters observed |
|
Didanosine 200 mg every 12 hours simultaneously administered with ganciclovir |
5 mg/kg IV twice daily |
11 |
No effect on ganciclovir PK parameters observed |
|
5 mg/kg IV once daily |
|||
|
Probenecid 500 mg every 6 hours |
1000 mg orally every 8 hours |
10 |
AUC ↑53 ± 91% (range: -14% to 299%) Ganciclovir renal clearance ↓22 ± 20% (range: -54% to -4%) |
|
Coadministered Drug |
Ganciclovir Dosage |
N |
Coadministered Drug Pharmacokinetic (PK) Parameter |
|
Oral cyclosporine at therapeutic doses |
5 mg/kg infused over 1 hour every 12 hours |
93 |
In a retrospective analysis of liver allograft recipients, there was no evidence of an effect on cyclosporine whole blood concentrations. |
|
Mycophenolate mofetil (MMF) 1.5 g single dose |
5 mg/kg IV single dose |
12 |
No PK interaction observed (patients with normal renal function) |
|
Trimethoprim 200 mg once daily |
12 |
No effect on trimethoprim PK parameters observed. |
|
|
Didanosine 200 mg every 12 hours |
5 mg/kg IV twice daily |
11 |
AUC 0-12↑70 ± 40% (range: 3% to 121%) C max↑49 ± 48% (range: -28% to 125%) |
|
Didanosine 200 mg every 12 hours |
5 mg/kg IV once daily |
11 |
AUC 0-12↑50 ± 26% (range: 22% to 110%) C max↑36 ± 36% (range: -27% to 94%) |
12.4 Microbiology
Mechanism of Action
Ganciclovir is a synthetic analogue of 2'-deoxyguanosine, which inhibits replication of human CMV in cell culture and in vivo. In CMV-infected cells, ganciclovir is initially phosphorylated to ganciclovir monophosphate by the viral protein kinase, pUL97. Further phosphorylation occurs by cellular kinases to produce ganciclovir triphosphate, which is then slowly metabolized intracellularly. As the phosphorylation is largely dependent on the viral kinase, phosphorylation of ganciclovir occurs preferentially in virus-infected cells. The virustatic activity of ganciclovir is due to inhibition of the viral DNA polymerase, pUL54, by ganciclovir triphosphate.
Antiviral Activity
The quantitative relationship between the cell culture susceptibility of human herpes viruses to antivirals and clinical response to antiviral therapy has not been established, and virus sensitivity testing has not been standardized. Sensitivity test results, expressed as the concentration of drug required to inhibit the growth of virus in cell culture by 50% (EC 50), vary greatly depending upon a number of factors including the assay used. Thus the median concentration of ganciclovir that inhibits CMV replication (EC 50value) in cell culture (laboratory strains or clinical isolates) has ranged from 0.08 to 13.6 μM (0.02 to 3.48 mcg/mL). Ganciclovir inhibits mammalian cell proliferation (CC 50value) in cell culture at higher concentrations ranging from 118 to 2840 μM (30 to 725 mcg/mL). Bone marrow-derived colony-forming cells are more sensitive [CC 50value = 0.1 to 2.7 μM (0.028 to 0.7 mcg/mL)]. The relationship between the antiviral activity in cell culture and clinical response has not been established.
Viral Resistance
Cell Culture
CMV isolates with reduced susceptibility to ganciclovir have been selected in cell culture. Growth of CMV strains in the presence of ganciclovir resulted in the selection of amino acid substitutions in the viral protein kinase pUL97 and the viral DNA polymerase pUL54.
In Vivo
Viruses resistant to ganciclovir can arise after prolonged treatment or prophylaxis with ganciclovir by selection of substitutions in pUL97 and/or pUL54. Limited clinical data are available on the development of clinical resistance to ganciclovir and many pathways to resistance likely exist. In clinical isolates, seven canonical pUL97 substitutions, (M460V/I, H520Q, C592G, A594V, L595S, C603W) are the most frequently reported ganciclovir resistance-associated substitutions. These and other substitutions less frequently reported in the literature, or observed in clinical trials, are listed in Table 10.
|
pUL97 |
L405P, A440V, M460I/V/T/L, V466G/M, C518Y, H520Q, P521L, del 590-593, A591D/V, C592G, A594E/G/T/V/P, L595F/S/T/W, del 595, del 595-603, E596D/G/Y, K599E/M, del 600-601, del 597‑600, del 601-603, C603W/R/S/Y, C607F/S/Y, I610T, A613V |
|
pUL54 |
E315D, N408D/K/S, F412C/L/S, D413A/E/N, L501F/I, T503I, K513E/N/R, D515E, L516W, I521T, P522A/L/S, V526L, C539G, L545S/W, Q578H/L, D588E/N, G629S, S695T, I726T/V, E756K, L773V, V781I, V787L, L802M, A809V, T813S, T821I, A834P, G841A/S, D879G, A972V, del 981‑982, A987G |
CMV resistance to ganciclovir has been observed in individuals with AIDS and CMV retinitis who have never received ganciclovir therapy. Viral resistance has also been observed in patients receiving prolonged treatment for CMV retinitis with ganciclovir. In a controlled study of oral ganciclovir for prevention of AIDS-associated CMV disease, 364 individuals had one or more cultures performed after at least 90 days of ganciclovir treatment. Of these, 113 had at least one positive culture. The last available isolate from each subject was tested for reduced sensitivity, and 2 of 40 were found to be resistant to ganciclovir. These resistant isolates were associated with subsequent treatment failure for retinitis. The possibility of viral resistance should be considered in patients who show poor clinical response or experience persistent viral excretion during therapy.
Cross Resistance
Cross-resistance has been reported for amino acid substitutions selected in cell culture by ganciclovir, cidofovir or foscarnet. In general, amino acid substitutions in pUL54 conferring cross-resistance to ganciclovir and cidofovir are located within the exonuclease domains and region V of the viral DNA polymerase. Whereas, amino acid substitutions conferring cross-resistance to foscarnet are diverse, but concentrate at and between regions II (codons 696-742) and III (codons 805-845). The amino acid substitutions that resulted in reduced susceptibility to ganciclovir and either cidofovir and/or foscarnet are summarized in Table 11.
|
Cross-resistant to cidofovir |
D301N, N408D/K, N410K, F412C/L/S/V, D413E/N, P488R, L501I, T503I, K513E/N, L516R/W, I521T, P522S/A, V526L, C539G/R, L545S/W, Q578H, D588N, I726T/V, E756K, L773V, V812L, T813S, A834P, G841A, del 981-982, A987G |
|
Cross-resistant to foscarnet |
F412C, Q578H/L, D588N, V715A/M, E756K, L773V, V781I, V787L, L802M, A809V, V812L, T813S, T821I, A834P, G841A/S, del 981-982 |
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis, Mutagenesis
Ganciclovir was carcinogenic in mice at the same mean drug exposure in humans as at the RHD (5 mg/kg). At the dose of 1000 mg/kg/day (1.4 times the exposure at the RHD), there was a significant increase in the incidence of tumors of the preputial gland in males, forestomach (nonglandular mucosa) in males and females, and reproductive tissues (ovaries, uterus, mammary gland, clitoral gland and vagina) and liver in females. At the dose of 20 mg/kg/day (0.1 times the exposure at the RHD), a slightly increased incidence of tumors was noted in the preputial and harderian glands in males, forestomach in males and females, and liver in females. No carcinogenic effect was observed in mice administered ganciclovir at 1 mg/kg/day (exposure estimated as 0.01 times the RHD). Except for histiocytic sarcoma of the liver, ganciclovir-induced tumors were generally of epithelial or vascular origin. Although the preputial and clitoral glands, forestomach and harderian glands of mice do not have human counterparts, ganciclovir should be considered a potential carcinogen in humans.
Ganciclovir increased mutations in mouse lymphoma cells and DNA damage in human lymphocytes in vitro at concentrations between 50 to 500 and 250 to 2000 µg/mL, respectively. In the mouse micronucleus assay, ganciclovir was clastogenic at doses of 150 and 500 mg/kg (2.8 to 10 times the exposure at the RHD) but not at doses of 50 mg/kg (exposure approximately comparable to the RHD). Ganciclovir was not mutagenic in the Ames Salmonella assay at concentrations of 500 to 5000 µg/mL.
Impairment of Fertility
Ganciclovir caused decreased mating behavior, decreased fertility, and an increased incidence of embryolethality in female mice following doses of 90 mg/kg/day (exposures approximately 1.7 times the RHD). Ganciclovir caused decreased fertility in male mice and hypospermatogenesis in mice and dogs following daily oral or intravenous administration of doses ranging from 0.2 to 10 mg/kg. Systemic drug exposure (AUC) at the lowest dose showing toxicity in each species ranged from 0.03 to 0.1 times the exposure at the RHD.
14. Clinical Studies
14.1 Treatment of CMV Retinitis
In a retrospective, non-randomized, single-center analysis of 41 patients with AIDS and CMV retinitis diagnosed by ophthalmologic examination between August 1983 and April 1988, treatment with intravenous ganciclovir resulted in a delay in mean (median) time to first retinitis progression compared to untreated controls [105 (71) days from diagnosis vs. 35 (29) days from diagnosis]. Patients in this series received induction treatment of intravenous ganciclovir 5 mg/kg twice daily for 14 to 21 days followed by maintenance treatment with either 5 mg/kg once daily, 7 days per week or 6 mg/kg once daily, 5 days per week.
In a controlled, randomized study conducted between February 1989 and December 1990, immediate treatment with intravenous ganciclovir was compared to delayed treatment in 42 patients with AIDS and peripheral CMV retinitis; 35 of 42 patients (13 in the immediate-treatment group and 22 in the delayed-treatment group) were included in the analysis of time to retinitis progression. Based on masked assessment of fundus photographs, the mean [95% CI] and median [95% CI] times to progression of retinitis were 66 days [39, 94] and 50 days [40, 84], respectively, in the immediate-treatment group compared to 19 days [11, 27] and 13.5 days [8, 18], respectively, in the delayed-treatment group.
Data from trials ICM 1653, ICM 1774, and AVI 034, which were performed comparing intravenous ganciclovir to oral ganciclovir for treatment of CMV retinitis in patients with AIDS, are shown in Table 12, and Figures 1, 2, and 3, and are discussed below.
|
Demographics |
ICM 1653 (n=121) |
ICM 1774 (n=225) |
AVI 034 (n=159) |
|
|
Median age (years) Range |
38 |
37 |
39 |
|
|
24-62 |
22-56 |
23-62 |
||
|
Sex |
Males |
116 (96%) |
222 (99%) |
148 (93%) |
|
Females |
5 (4%) |
3 (1%) |
10 (6%) |
|
|
Ethnicity |
Asian |
3 (3%) |
5 (2%) |
7 (4%) |
|
Black |
11 (9%) |
9 (4%) |
3 (2%) |
|
|
Caucasian |
98 (81%) |
186 (83%) |
140 (88%) |
|
|
Other |
9 (7%) |
25 (11%) |
8 (5%) |
|
|
Median CD 4Count Range |
9.5 0-141 |
7.0 0-80 |
10.0 0-320 |
|
|
Mean (SD) Observation Time (days) |
107.9 (43.0) |
97.6 (42.5) |
80.9 (47.0) |
|
Trial ICM 1653
In this randomized, open-label, parallel group trial, conducted between March 1991 and November 1992, patients with AIDS and newly diagnosed CMV retinitis received a 3-week induction course of intravenous ganciclovir solution, 5 mg/kg twice daily for 14 days followed by 5 mg/kg once daily for 1 additional week. Following the 21-day intravenous induction course, patients with stable CMV retinitis were randomized to receive 20 weeks of maintenance treatment with either intravenous ganciclovir solution, 5 mg/kg once daily, or ganciclovir capsules, 500 mg 6 times daily (3000 mg/day). The study showed that the mean [95% CI] and median [95% CI] times to progression of CMV retinitis, as assessed by masked reading of fundus photographs, were 57 days [44, 70] and 29 days [28, 43], respectively, for patients on oral therapy compared to 62 days [50, 73] and 49 days [29, 61], respectively, for patients on intravenous therapy. The difference [95% CI] in the mean time to progression between the oral and intravenous therapies (oral - IV) was -5 days [-22, 12]. See Figure 1for comparison of the proportion of patients remaining free of progression over time.
Trial ICM 1774
In this three-arm, randomized, open-label, parallel group trial, conducted between June 1991 and August 1993, patients with AIDS and stable CMV retinitis following from 4 weeks to 4 months of treatment with intravenous ganciclovir solution were randomized to receive maintenance treatment with intravenous ganciclovir solution, 5 mg/kg once daily, ganciclovir capsules, 500 mg 6 times daily, or ganciclovir capsules, 1000 mg three times daily for 20 weeks. The study showed that the mean [95% CI] and median [95% CI] times to progression of CMV retinitis, as assessed by masked reading of fundus photographs, were 54 days [48, 60] and 42 days [31, 54], respectively, for patients on oral therapy compared to 66 days [56, 76] and 54 days [41, 69], respectively, for patients on intravenous therapy. The difference [95% CI] in the mean time to progression between the oral and intravenous therapies (oral - IV) was -12 days [-24, 0]. See Figure 2for comparison of the proportion of patients remaining free of progression over time.
Trial AVI 034
In this randomized, open-label, parallel group trial, conducted between June 1991 and February 1993, patients with AIDS and newly diagnosed (81%) or previously treated (19%) CMV retinitis who had tolerated 10 to 21 days of induction treatment with intravenous ganciclovir, 5 mg/kg twice daily, were randomized to receive 20 weeks of maintenance treatment with either ganciclovir capsules, 500 mg 6 times daily or intravenous ganciclovir solution, 5 mg/kg/day. The mean [95% CI] and median [95% CI] times to progression of CMV retinitis, as assessed by masked reading of fundus photographs, were 51 days [44, 57] and 41 days [31, 45], respectively, for patients on oral therapy compared to 62 days [52, 72] and 60 days [42, 83], respectively, for patients on intravenous therapy. The difference [95% CI] in the mean time to progression between the oral and intravenous therapies (oral - IV) was -11 days [-24, 1]. See Figure 3for comparison of the proportion of patients remaining free of progression over time.
Comparison of other CMV retinitis outcomes between oral and IV formulations (development of bilateral retinitis, progression into Zone 1, and deterioration of visual acuity), while not definitive, showed no marked differences between treatment groups in these studies. Because of low event rates among these endpoints, these studies are underpowered to rule out significant differences in these endpoints.
Figure 1. ICM 1653: Time to Progression of CMV Retinitis
Figure 2. ICM 1774: Time to Progression of CMV Retinitis
Figure 3. AVI 034: Time to Progression of CMV Retinitis
14.2 Prevention of CMV Disease in Transplant Recipients
Intravenous ganciclovir was evaluated in three randomized, controlled trials of prevention of CMV disease in organ transplant recipients.
Trial ICM 1496
In a randomized, double-blind, placebo-controlled study of 149 heart transplant recipients at risk for CMV infection (CMV seropositive or a seronegative recipient of an organ from a CMV seropositive donor), there was a reduction in the overall incidence of CMV disease in patients treated with intravenous ganciclovir. Immediately post-transplant, patients received intravenous ganciclovir solution 5 mg/kg twice daily for 14 days followed by 6 mg/kg once daily for 5 days/week for an additional 14 days. Twelve of the 76 (16%) patients treated with intravenous ganciclovir vs. 31 of the 73 (43%) placebo-treated patients developed CMV disease during the 120-day post-transplant observation period. No significant differences in hematologic toxicities were seen between the two treatment groups [see Adverse Reactions (6.1)].
Trial ICM 1689
In a randomized, double-blind, placebo-controlled study of 72 bone marrow transplant recipients with asymptomatic CMV infection (CMV positive culture of urine, throat or blood) there was a reduction in the incidence of CMV disease in patients treated with intravenous ganciclovir following successful hematopoietic engraftment. Patients with virologic evidence of CMV infection received intravenous ganciclovir solution 5 mg/kg twice daily for 7 days followed by 5 mg/kg once daily through day 100 post-transplant. One of the 37 (3%) patients treated with intravenous ganciclovir vs. 15 of the 35 (43%) placebo-treated patients developed CMV disease during the study. At 6 months post-transplant, there continued to be a reduction in the incidence of CMV disease in patients treated with intravenous ganciclovir. Six of 37 (16%) patients treated with intravenous ganciclovir vs. 15 of the 35 (43%) placebo-treated patients developed disease through 6 months post-transplant. The overall rate of survival was higher in the group treated with intravenous ganciclovir, both at day 100 and day 180 post-transplant. Although the differences in hematologic toxicities were not statistically significant, the incidence of neutropenia was higher in the group treated with intravenous ganciclovir [see Adverse Reactions (6.1)].
Trial ICM 1570
This was a randomized, unblinded study that evaluated 40 allogeneic bone marrow transplant recipients at risk for CMV disease. Patients underwent bronchoscopy and bronchoalveolar lavage (BAL) on day 35 post-transplant. Patients with histologic, immunologic or virologic evidence of CMV infection in the lung were then randomized to observation or treatment with intravenous ganciclovir solution (5 mg/kg twice daily for 14 days followed by 5 mg/kg once daily 5 days/week until day 120). Four of 20 (20%) patients treated with intravenous ganciclovir and 14 of 20 (70%) control patients developed interstitial pneumonia. The incidence of CMV disease was lower in the group treated with intravenous ganciclovir, consistent with the results observed in ICM 1689.
16. How is Ganciclovir supplied
How Supplied
Ganciclovir for Injection, USP is supplied in 10 mL sterile single-dose vials, each containing 543 mg ganciclovir sodium equivalent to 500 mg of ganciclovir as a white to off-white powder. The concentration of ganciclovir in the reconstituted solution is 50 mg/mL. Because ganciclovir shares some of the properties of antitumor agents (i.e., carcinogenicity and mutagenicity), consideration should be given to handling and disposal according to guidelines issued for antineoplastic drugs. Ganciclovir for Injection, USP is supplied in cartons of 25 vials (NDC 70436-231-55).
Storage
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [See USP Controlled Room Temperature].
Store reconstituted solution in the vial at 25°C (77°F) for no longer than 12 hours. Do not refrigerate or freeze. Discard any unused portion of the reconstituted solution.
Store diluted infusion solution under refrigeration at 2° to 8°C (36° to 46°F) for no longer than 24 hours. Do not freeze.
17. Patient Counseling Information
Hematologic Toxicity
Inform patients that ganciclovir may cause hematologic toxicity including granulocytopenia (neutropenia), anemia, and thrombocytopenia. Inform patients that their blood counts and platelet counts should be closely monitored while on treatment [see Warnings and Precautions (5.1)].
Impairment of Renal Function
Inform patients that ganciclovir has been associated with decreased renal function and that serum creatinine or creatinine clearance should be monitored while on treatment to allow for dosage adjustment in patients with renal impairment [see Warnings and Precautions (5.2)].
Impairment of Fertility
Inform patients that ganciclovir may cause temporary or permanent infertility in humans [see Warnings and Precautions (5.3), Use in Specific Populations (8.3)].
Pregnancy and Contraception
Advise female patients to use effective contraception during and for at least 30 days following treatment with ganciclovir for injection. Similarly, advise men to practice barrier contraception during and for at least 90 days following treatment with ganciclovir for injection [see Warnings and Precautions (5.4), Use in Specific Populations (8.1, 8.3)].
Carcinogenicity
Inform patients that ganciclovir should be considered a potential carcinogen [see Warnings and Precautions (5.5)].
Drug Interactions
Inform patients that ganciclovir for injection may interact with other drugs. Advise patients to report to their healthcare provider the use of any other medication [see Drug Interactions (7)].
Impairment of Cognitive Ability
Based on the adverse reaction profile, ganciclovir may affect cognitive abilities, including the ability to drive and operate machinery, as seizures, dizziness, and/or confusion have been reported with the use of ganciclovir [see Adverse Reactions (6.1)].
Opthalmological Examination in Patients with CMV Retinitis
Inform patients that ganciclovir is not a cure for CMV retinitis, and they may continue to experience progression of retinitis during or following treatment. Advise patients to have frequent ophthalmological follow-up examinations while being treated with ganciclovir for injection. Some patients may require more frequent ophthalmological follow-up [see Dosage and Administration (2.2), Adverse Reactions (6.1)].
Lactation
Advise nursing mothers not to breastfeed if they are receiving ganciclovir for injection because of the potential for serious adverse events in nursing infants and because HIV can be passed to the baby in breast milk [see Use in Specific Populations (8.2)].
Rx only
Manufactured by:
Hainan Poly Pharm Co., Ltd., Guilinyang Economic Development Zone, Haikou, Hainan, China 571127
Distributed by:
Slate Run Pharmaceuticals, LLC, Columbus, Ohio 43215
10000485/01
Revised: 05/2024
| GANCICLOVIR SODIUM
ganciclovir sodium injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Slate Run Pharmaceuticals, LLC (039452765) |
| Registrant - Hainan Poly Pharm. Co., Ltd. (654561638) |
More about ganciclovir
- Check interactions
- Compare alternatives
- Pricing & coupons
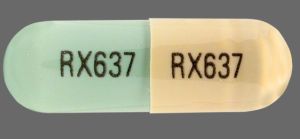
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: purine nucleosides
- Breastfeeding
- En español
Patient resources
- Ganciclovir injection drug information
- Ganciclovir (Oral, Intravenous) (Advanced Reading)
- Ganciclovir (Systemic)